|
As the world's governments raced to deal with a looming flu pandemic starting some two weeks ago, in late April 2009, World Health Organisation (WHO) officials confirmed that the world is better prepared than ever before to deal with a pandemic, thanks largely to six years of research and preparations to battle bird flu and SARS. Nearly 150 countries are now known to have drawn up contingency plans covering everything from the response of health services to travel restrictions and international co-operation.
Although it contains animal genetic components, the current influenza A(H1N1) virus has not been diagnosed in animals before and has spread from person to person, threatening an influenza pandemic which, according to scientists, is inevitable, even though no one can predict the timing. Three serious influenza pandemics occurred in the 20th century, with each new virus eventually infecting up to a third of the world over the course of one to two years: the 1918 ‘Spanish flu’ responsible for more than 40 million deaths, followed by the 1957 ‘Asian’ and 1968 ‘Hong Kong flu’, which killed between 1 and 3 million people worldwide,
The history of flu epidemics and pandemics, which can be traced back with some accuracy for the past 300 years, tells us that outbreaks occur somewhere in the world in most years and pandemics, which are epidemics that spread worldwide, at 10- to 50-year intervals. Despite influenza and its causative organism being the most studied of viral diseases and pathogens until the advent of HIV/AIDS two decades ago, little has been done in the past century to change the pattern of influenza infections.
|
2009 June 11 Swine flu update:
-
WHO on 11 June raised the pandemic alert level from phase 5 to 6, indicating a global pandemic outbreak
-
This will trigger drug makers to speed production of a swine flu vaccine and prompt governments to devote more money to containing the virus.
-
Although appearing less deadly than seasonal flu, experts worry the virus could mutate into a more lethal strain during the Southern Hemisphere’s coming flu season.
-
Experts also worry that poorer countries could be overwhelmed with cases they do not have the capacity to treat.
-
The last pandemic, the Hong Kong flu of 1968, killed 700,000 people worldwide. Ordinary flu kills 250,000 to 500,000 people each year
|
|
11 May 2009 brief from the World Health Organisation
For more information, we encourage our readers to read the WHO brief copied below and linked to here:
http://www.who.int/csr/disease/swineflu/assess/disease_swineflu_assess_20090511/en/index.html
This WHO brief of 11 May 2009 provides much useful background information for understanding expert concerns about the current new flu virus, particularly how it may affect the developing countries of the southern hemisphere, where the flu season is about to begin. These expert concerns include the following.
-
The influenza A(H1N1) could mutate into a more lethal form in a subsequent wave of this pandemic, as the virus causing the 1918 pandemic flu did.
-
Having not appeared in humans or animals before, scientists anticipate that pre-existing immunity to the virus will be low or non-existent, or largely confined to older population groups that have had flu vaccinations and therefore striking down more people of a younger age group, than viruses causing normal so-called 'seasonal flu'.
-
This new flu virus, although as yet causing generally mild illness in the 29 countries outside Mexico where it has so far been confirmed, could cause severe illness in developing countries, particularly:
• people suffering malnutrition
• poor communities with inadequate health care
• the greatly increased numbers of people now afflicted with chronic conditions such as heart disease and diabetes, conditions that can greatly increase the severity of illness this flu causes (although these chronic conditions afflicted mostly affluent populations until a few decades ago, a full 85% of people suffering them today live in low- and middle-income countries)
-
As this new influenza A(H1N1) virus spreads to the southern hemisphere with the start of the flu season here, it may meet the H5N1 bird flu virus that is widely circulating among the poultry populations of some developing countries; no one knows how, under pressure of the new A(H1N1) human-to-human transmitted flu virus, the H5N1 bird-to-bird transmitted flu virus might change, including whether the latter, more lethal, bird flu virus could be helped to mutate into a form transmitted easily among people. (The more lethal H5N1 bird flu virus, now endemic in many areas, has thankfully to date been transmitted only rarely directly from person to person; almost all the people infected have received the virus from handling infected poultry, which has helped keep the virus from spreading widely among human populations.)
|
|
11 May 2009 Update
11 May 2009 Update As reported in Time Magazine this week (11 May 2009), ‘new research suggests that the WHO acted wisely in raising the pandemic alarm — and that the threat of H1N1 may not have passed. In a study released May 11 in the journal Science, researchers from Imperial College London, along with WHO staff and Mexican scientists, conclude that H1N1 is transmitted considerably easier than the regular seasonal flu and is about as deadly as the 1957 Asian flu, which killed about 2 million people worldwide. A World Bank study last year found that a pandemic of similar severity today might kill 14.2 million people around the world, and cut 2% from the global economy.’
|
|
7 May 2009 Update
As of 7 May 2009, there were 2,371 confirmed cases of swine flu in 24 countries and 46 deaths from this infection, all but 2 of the deaths occurring in Mexico. Scientists described 11 cases of Americans who were infected before the current outbreak with swine flus that partly matched the new epidemic strain that emerged in Mexico in March 2009. The first case was in December 2005. In articles published online in The New England Journal of Medicine, virologists from the US Centers for Disease Control and Prevention (CDC) described those cases, most of them in young people in the Midwest who touched or were near pigs. All had a ‘triple reassortant’ virus that combined human, swine and avian flu genes. The H1N1 flu now spreading out from Mexico also has those genes, as well as genes from Eurasian swine. The CDC reports that the pandemic does not appear to be petering out, that we appear to be still on the upswing of the epidemic curve, and that only about 10% of those infected had a travel history to Mexico.
|
The role of livestock scientists in the developing world
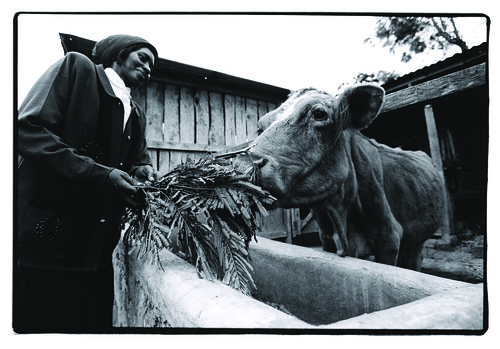
Livestock scientists have a vital role to play in helping to predict, prevent and control zoonotic diseases, which are all those transmitted between animals and people. Remarkably, zoonoses make up more than 60% of all human infectious diseases and more than 70% of all emerging infectious diseases. These diseases occur most frequently in Asia and Africa, where limited resources hinder both surveillance and response. The growing threat of emerging diseases such as Nipah and SARS, and re-emerging diseases such as Rift Valley Fever and avian influenza, has served as a wakeup call to animal health and public health services that their collaboration is necessary if these threats are to be minimized. There is increasing recognition that, for a number of zoonotic diseases, the most effective way to protect the health of the public is to control disease in the animal host.
The work of livestock scientists working in and for developing countries has special relevance in tackling these animal-human diseases, because within developing countries today, fast changes in food systems wrought by skyrocketing demand for, and production of, livestock foods is creating new niches and transmission pathways for pathogens, with unprecedented numbers of diseases emerging and re-emerging in recent decades. New tools and approaches for managing diseases in developing countries are urgently needed.
|
The animal-human disease interface
Most pathogens (61%) that affect people also affect animals; such shared infecting organisms and infections are known as ‘zoonotic’. A full 71% of all the world’s emerging infectious diseases are zoonotic, or transmissible between people and animals. In addition to swine flu, bird flu and SARS, these diseases include such devastating plagues as BSE (mad cow disease), HIV/AIDS, ebola and Rift Valley fever. The bugs that cause these diseases are notorious for their ability to evolve. Flu viruses, for example, can change both from severe to mild and from mild to severe.
|
Researchers at ILRI have been working at the livestock-human disease interface, supporting better integration of veterinary and public health surveillance programs, for three decades. ILRI’s particular interests are aspects of zoonotic diseases that impact the world’s poorest communities, where animal husbandry is a way of life and a central means of livelihood for more than half a billion people. ILRI and its partners, for example, make evidence-based assessments of the different impacts on the poor of employing different disease-control methods, thereby helping policymakers determine optimal pro-poor strategies for different regions and agricultural production systems of the developing world.
ILRI works with many research institutions within developing countries to better control zoonotic diseases at local, national and regional levels. It works with WHO and its international network of institutions to bolster disease surveillance. It works with the World Organisation for Animal Health (OIE) and the Food and Agriculture Organization of the United Nations (FAO) on participatory epidemiology, a grassroots approach to disease surveillance and control that is being successfully applied in the battle against bird flu in Indonesia. And it works with regional agencies such as the Africa Union / Inter-African Bureau for Animal Resources to improve laboratory testing and diagnosis of bird flu and other infectious livestock diseases.
ILRI and its partners are also investigating risk-based approaches that focus on key hazards and maximize benefits with available resources. With case studies in Africa and Asia, and concepts derived from ‘one medicine’ and ‘one health’, ILRI scientists argue that a ‘risk-analysis framework’ both can and should be extended to integrate risks to animal, human and environmental health.
The role of policy
ILRI also works with the International Food Policy Research Institute (IFPRI) and other institutions on providing evidenced-based policy support so that we don’t fall into the trap of doing more harm than good in our efforts to control infections, particularly in poor countries which can least afford such mistakes.
Some of the most profound consequences of disease threats are economic rather than medical, with inappropriate policies devastating local and national economies. Egypt’s on-going culling of its entire population of some 300,000 pigs, for example, is reported to be reigniting religious and economic tensions, and may end up doing more harm than good. The pigs are kept not by Egypt’s majority Muslim population, which views the animals as unclean, but by Egypt’s Coptic Christians, many of whom maintain pigs on the rubbish heaps of shantytowns, where entire families pick out organic waste to feed their pigs. On the other hand, Egyptian authorities may be trying to prevent a repeat of events two years ago, when they were criticized for not responding swiftly enough to an outbreak of bird flu, which killed 26 people in the country, three in just the last month.
‘Misconceptions and inappropriate responses can spread quickly during the early stages of a new disease outbreak,’ says John McDermott, a veterinary epidemiologist and ILRI’s director of research. ‘This “swine flu” is spread by people, not by pigs,’ he said. ‘So most authorities are appropriately focusing their current attention on stopping the spread of swine flu among people.’ (Bird flu, in contrast, is spread by birds, so authorities focus on controlling that disease within poultry rather than human populations.) This new swine flu virus, and our reactions to it, like the more lethal bird flu and SARS before it, should provide us with many lessons for the future.
Research gaps
We still know little about the nature of this new influenza virus strain, other than its genetic makeup is a ‘mashup’ of human, bird and pig elements (making the name ‘swine flu’ something of a misnomer we shall probably have to live with; ‘Spanish flu’ didn’t originate in Spain, but the name stuck anyhow). We don’t know yet when it first made the jump from pig to person, why it has been so deadly in Mexico but not elsewhere, or how virulent it will eventually prove to be. The pathogenicity of a virus can become milder or more severe over time. Until now, the influenza A(H1N1) virus thankfully has proven relatively mild, with most of those infected responding well to usual flu treatments and recovering.
Our ignorance of this new strain of swine flu virus is partly due to our neglect of animal health matters. In rich as well as poor countries, veterinary health care and research remains chronically under-funded. And there is increasing need for disease control policymakers, agents and researchers to collaborate at the interface of the human-and-animal-health sectors, exchanging up-to-date information on disease outbreaks and transmission.
Controlling emerging infectious diseases
‘To get serious about preventing new zoonotic infections from spreading,’ says Carlos Seré, director general of the Africa-based International Livestock Research Institute (ILRI), ‘we need to get serious about veterinary resources. We need new ways to look for new pathogens infecting animals, new ways to assess those which may be most dangerous, and new ways to determine how they may be transmitted to people. We have just had a demonstration as to the danger of waiting for a new flu to emerge and begin spreading among people before trying to contain it.’
The influenza A(H1N1) virus is spreading rapidly because in our ever-shrinking, ever-globalizing world, pathogens are crossing species and borders with increasing ease. In such a world, says Seré, ‘we ignore veterinary health problems in developing countries at our peril.’ With high-quality collaboration among countries (rich and poor alike), scientific disciplines (e.g. socio-economics as well as genetics), and sectors (e.g. medical, veterinary, agricultural, environmental, wildlife), Seré argues, we can manage today’s emerging disease threats.
Because animals are the origin of most emerging diseases, they could play the same role that canaries did in the mines, in that case, alerting the coal workers to the presence of noxious gases or too little oxygen.
‘We should be spotting many infectious disease threats not in people, as we did in the case of this new flu virus,’ says Seré, ‘but rather in animal populations.’ That should give authorities more time to design and implement interventions to protect people from becoming infected. ‘But as we’ve seen in recent outbreaks of bird flu and Rift Valley fever, all too often it is people rather than animals that serve as our sentinels, sickening and dying after the disease has begun circulating in local livestock populations.’ That’s largely because in poor countries, livestock diseases tend to go unreported (it’s hard to tell one livestock disease from another in countries with spotty veterinary coverage) and/or underappreciated (people facing serious human health problems have little time to spare worrying about animal diseases), and/or ignored (it may be considered political suicide to report a disease outbreak that might have large economic consequences).
‘To find better ways of controlling human diseases,’ Seré concludes, ‘we’re going to have to find better ways of understanding and controlling diseases in both domesticated and wild animal populations. And we’re all going to have to work together, breaking down traditional barriers between organizations and scientific disciplines in the process. We need new thinking to tackle these new threats. And bringing diverse expertise together is the best way of staying on top of fast-evolving situations that threaten our global public health—as well as the well being of the world’s poorer livestock keeping communities.’
For more information contact
John Mc Dermott
Deputy Director General-ILRI
Nairobi, Kenya
Email: j.mcdermott@cgiar.org
Telephone: +254 20 422 3207
|


 This
This 
